Wisdom Teeth
Wisdom teeth, or third molars, are the last teeth to develop and may or may not erupt into the mouth. When they align properly and the surrounding gum tissue is healthy, they do not have to be removed. Unfortunately, this is not common. When a wisdom tooth is unable to fully erupt into the mouth, it is said to be impacted. In general, impacted third molars can be partially or fully impacted usually because there is not enough space for the wisdom tooth to erupt behind the second molars. Most people have at least one impacted wisdom tooth.
The clinical and radiographic information for each patient is applied to critically weigh your treatment options. A course of action that best fits the needs of you, the patient, will be discussed. Appropriate treatment options may include removal, partial removal (coronectomy), or leaving the wisdom tooth in place.
Wisdom teeth that are completely erupted and functional, painless, free of caries, with healthy gum tissue, and without other associated pathologic conditions may not require extraction. They do however, require hygiene maintenance and periodic clinical and radiographic surveillance if left in place.
Why Should I Remove My Wisdom Teeth?
The removal of third molar teeth is always appropriate when there is evidence of pathological changes such as gum disease, non-restorable carious lesions, infection, cysts, tumors, and damage to adjacent teeth. The medical necessity for removal of erupted, partially visible, and fully impacted third molar teeth that are asymptomatic can also be justified, as there can still be disease without symptoms or to prevent future problems.
Studies have documented the presence of gum disease around even asymptomatic third molars. Studies show an association between third molar teeth and gum disease in both younger and older patient populations. Patients more than 25 years old had greater gum pocketing associated with their third molars.
Research has also shown that erupted third molar teeth are as likely to have an increased frequency of gum disease as impacted third molars. These studies and others show that patients with wisdom teeth that have no symptoms may actually have active inflammatory periodontal disease. There is supporting evidence that once gum or pericoronal disease is established in the third molar areas, the problem can be persistent and progressive, but improves following extraction of the wisdom teeth.
Pericoronal gum infections commonly occur around wisdom teeth in which trapped food debris contributes to bacterial growth and infection. The resultant pain from these infections causes patients to seek care. The presence of a symptomatic or asymptomatic pericoronal infection is an absolute indication for removal of the third molar teeth. Periodontal pocketing and the presence of pericoronal infection are all indications that disease exists.
The extraction of wisdom teeth after the age of 25 can be a risk factor for incomplete healing and the need for additional treatment. Research supports the surgical intervention or removal of third molar teeth early, prior to the development of gum disease, when the post-surgical healing is optimal, and the risk of post-operative complications are lowest.
The elective, therapeutic removal of impacted wisdom teeth is recommended for teeth that are not likely to erupt into a disease free position and preferably before the onset of gum disease. There are other conditions in which extraction is recommended such as third molar tooth which is poorly positioned such that it prevents the eruption of an adjacent tooth, or causes damage to an adjacent tooth.
Cystic disease changes were found to be present in about one third of impacted third molars in one study. Dentigerous cysts associated with impacted third molar teeth are commonly asymptomatic. In these cases, the third molar tooth may be asymptomatic, but the overall condition is not disease free.
Jaw growth and the eruption pattern of third molar teeth may not be entirely predictable. There may or may not be adequate jaw length to accommodate the third molars. Wisdom teeth have been shown to continue to change in position over time within the mandible, generally to a less favorable position with respect to the difficulty in extraction and risk of intra-operative complications. The state of root development must also be considered, as the incidence of nerve injuries is statistically related to the age of the patient. A higher incidence of nerve injury in older patients has been attributed to more fully developed third molar root and third molars with roots in proximity to the inferior alveolar nerve. A decrease in nerve regeneration or neuronal plasticity is seen in older patients. Therefore the earlier removal of third molars is the usually the best treatment option.
Dr. Henry will evaluate the position of your wisdom teeth clinically with an oral and radiographic examination. He will discuss with you if there are present or future problems to be anticipated with your third molars. Patients are generally first evaluated during their teenage years.
The Removal Of Wisdom Teeth
The removal of wisdom teeth can be performed utilizing a variety of different anesthetic techniques including local anesthesia, with or without nitrous oxide conscious sedation, and/or intravenous anesthetic agents. These options as well as the surgical and anesthesia risks will be discussed with you before the procedure Is performed.
Dr. Henry and his staff have the training, and experience to provide various types of anesthesia to maximize your comfort. Surgery is usually performed in the office with appropriate anesthesia monitoring to provide patient safety. Outpatient surgery at the Cheshire Medical Center in Keene, NH may also be warranted in selective cases for a variety of reasons, and can be arranged for patient safety and management.
Once the teeth are extracted, written home care instructions regarding post-operative recovery care including, diet, activity, oral hygiene, and medications will be reviewed. Any post-operative questions or concerns regarding recovery will be answered at the time of surgery, by phone, or by follow-up post-operative office visit.
The early extraction of wisdom teeth is recommended to minimize the complications of gum infections, decay or damage to adjacent teeth, and the development of other pathological conditions such as cysts or tumors. Post-operative recovery can also be more difficult with increasing age, and the risk of complications has been shown to be more frequent in older patients.
In summary, the decision regarding the why, when or how to treat wisdom teeth has many considerations. These considerations include the presence of the third molar teeth, their position within the jaws, the condition of the teeth and adjacent teeth and structures, and the presence or potential for infection or pathology.
Thus the decision to remove wisdom teeth is done to help alleviate present disease or prevent future problems.
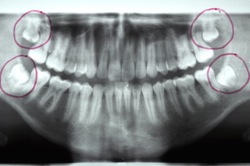
Four Impacted Third Molars

Cystic enlargement of follicular sac of implacted third molar displacing the tooth.
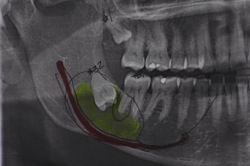
Cyst associated with impacted third molar displacing the inferior alveolar nerve.